DVT ICD 10
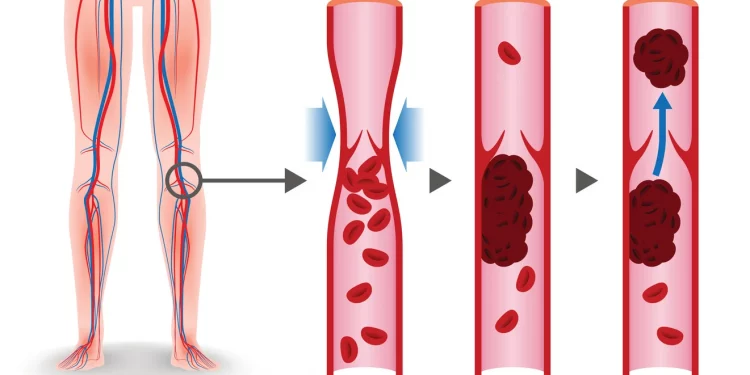
DVT ICD 10 – A deep vein thrombosis is a blood clot in a vein. It is usually located in the thigh or lower leg. Another name for the condition is thrombophlebitis. The diagnostic code for this condition is I82. 502, and it can be used for reimbursement purposes. The diagnosis is described by the physician and is based on the patient’s symptoms, medical history, and laboratory data.
Sensitivity
The sensitivity of ICD-10 to diagnose DVT was determined by comparing the PSI of the same diagnosis with the PSIs of chart review data. While low PPV PSIs can be useful in detecting cases, their sensitivity is low. It is difficult to determine the sensitivity of these PSIs because they are difficult to characterize. A recent study by Quan et al21 examined the effects of ICD-10 implementation on data quality. They found that the sensitivity was lower for seven conditions in ICD-10 data, while similar for the ICD-9-CM.
The sensitivity of ICD-10 codes for isolated DVT and PE was 58.0% and 88.9%, respectively. However, sensitivity varied widely, with median values ranging from 48.6 to 66.7 and 84.3% (108/128), respectively. Sensitivity was also lower in patients who had undergone surgery or were hospitalized. However, the sensitivity was still higher than those for PE.
The sensitivity of ICD-10 codes for DVT was determined using the Swedish National Procedural Reporting and Evaluation (NPR) database. The study evaluated a population-based random sample of patients with RA. Ethical approval was granted by the Swedish Regional Ethics Committee. In addition to the sensitivity of the codes, the PPV was also calculated. These values are important for identifying patients with DVT and PE.
The sensitivity of ICD-10 codes for DVT and PE was determined using hospital discharge diagnosis data. In a study that included 25 hospitals in France, ICD-10 codes identified a significant proportion of patients who had acute symptomatic DVT or PE that were later confirmed through objective testing. Using hospital discharge data to identify DVT and PE may reduce the rate of incorrect diagnosis. In addition, the use of ICD-10 codes in conjunction with imaging procedures can detect postoperative pulmonary embolism and acute venous thrombosis.
PPV
PPV of diagnosis of CVST in ICD-10-CM is good to excellent. However, some of the ICD-10-CM codes have a poor PPV, like I629. This has led to calls for more improvement in PPV and the addition of anticoagulants to case definitions. Here, we present a study that examines the PPV of PSIs for CVST in ICD-10-CM data in Canada.
We evaluated PPV for the diagnosis of PE/DVT by calculating the proportion of confirmed diagnosis compared to the number of participants in the registries. For example, PPV of PSI 12-PE/DVT ranged from 22% to 79%, across studies in the USA.
In addition, we performed a separate analysis of PPV for the two PSIs for this disease, focusing on the time period between January 1, 2009, and September 5, 2014.
The authors also examined the PPV of case definitions for pulmonary embolism in the National Health Insurance claims database in Taiwan, using ICD-10-CM diagnostic codes for CVST. Chang Gung Medical Foundation evaluated medical records and images to calculate the PPV of various case definitions of CVST. They found that patients with a history of VTE had higher PPVs than those without it.
The PPV of PE and DVT is extremely variable and varies greatly between diagnosis categories. The PPV for atrial fibrillation and herpes simplex encephalitis ranges from 79% to 100%. However, the PPV for secondary diagnoses falls within the same range, and this variation is likely due to differences in coding algorithms, registries, and patient populations.
Area Under the Receiver-Operating-Characteristic Curve (AUC)
The authors of this study used the Area Under the Receiver-Operating Characteristic Curve (AUC) of DVP to identify patients who would die in hospital. Patients with high D-dimer levels, elevated troponin T levels, and a sPESI score had a higher risk for inhospital mortality. The study’s sensitivity and specificity thresholds were 0.43 for Ddimer levels and 0.414 for sPESI scores, respectively.
The MIMIC-III database includes information about the mortality rates of patients in the ICU. The database contains scores for early mortality, current lower-limb paralysis, active cancer, and intensive care unit stays. The AUC-ROC curve and other clinical measures are used to compare these scores to the MIMIC-III score for DVT.
The AUC-ROC curves of the DVT icd-10 were also validated externally using the eICU dataset. Also the AUC-ROC curves of these two datasets were 0.86, 0.76, and 0.73, respectively. This suggests that the predictive model is accurate in predicting early mortality for patients with DVT.
Patient screening
This study used a multicenter cohort study to investigate the impact of a DVT screening programme on the incidence of pulmonary embolism. The programme was implemented at Uppsala University Hospital, a tertiary care hospital in Sweden. The programme involved online educational modules and a single hands-on session. The screening protocol was approved by the National Ethical Review Agency and written informed consent was obtained from all patients. In case of a refusal to give consent, next of kin was contacted.
This study found that DVT ICDM-VICD-10 codes had a satisfactory sensitivity and specificity in detecting PE and isolated DVT. It also showed that a substantial proportion of DVT cases are missed by using ICD-10 data for complication screening and research. However, there are several limitations to this study. This study used a limited sample size, and not all patients were eligible to participate. There may have been selection bias in the study, since a PE patient was excluded, and some patients were diagnosed with DVT at a later time.
This study also found that ICU residents with little or no DVT experience were capable of detecting DVT in critically ill patients with COVID-19. Furthermore, VTE was associated with an increased inflammatory response and hypercoagulation. These results suggest that point-of-care ultrasound screening of DVT may be a resource-saving alternative to expert CDUS. We thank Joanna Wessbergh, Erik Danielsson, and Philip Karlsson for their technical assistance. Furthermore, we thank Anna Gradin, Sten Rubertsson, and Tomas Luther for their input and support.
If you are unsure of whether the test code you receive will be accepted by the thirdparty payer for your DVT treatment, you can look at coding guidance for similar situations. This will help you determine whether you will receive reimbursement if your test is positive. The codes are updated as new information becomes available. And remember to check with your provider to make sure that you get the most reimbursement for your treatment. You’ll never know when the doctor may change their criteria, so don’t assume that a positive result means that you’ll get a full reimbursement for the procedure.
Comorbidities
In this study, the incidence of DVT was compared between patients with ESRD and controls without ESRD. Patients were matched according to age, lovemaking, and year of admission to the hospital. Patients were followed until DVT or death or withdrawal from the NHI. In addition, comorbidities were analyzed from outpatient records and 1 year before the index date.
The authors of this study analyzed data from the International Classification of Diseases and Injuries, using a Nationwide Inpatient Sample (NiS) and stratified probability sample of 20% of inpatient discharges. These samples are representative of more than 97% of the population. They used the ICD-10 codes for DVT and PE to estimate national incidence rates. The statistical significance of the results was determined using the Mann-Whitney U test.
Among DVT patients, hypertension and chronic pulmonary disease were the most common comorbidities. PE patients were twice as likely as those without chronic pulmonary disease to have comorbidities. Those with severe comorbidity were twice as likely to be hospitalized and die within a year. However, those with chronic pulmonary disease were also three times as likely to die. Consequently, patients with DVT or PE had a higher mortality risk than patients without these comorbidities.
People with severe comorbidities were more likely to have VTE. However, they were more likely to have a history of VTE. Those with a family history of the disease were at higher risk for developing VTE, as were those with a low educational level. Although the cause of the comorbidities was not determined, the study demonstrated that people with certain comorbidities had a higher risk of developing VTE than patients without such conditions.